Utilization
-
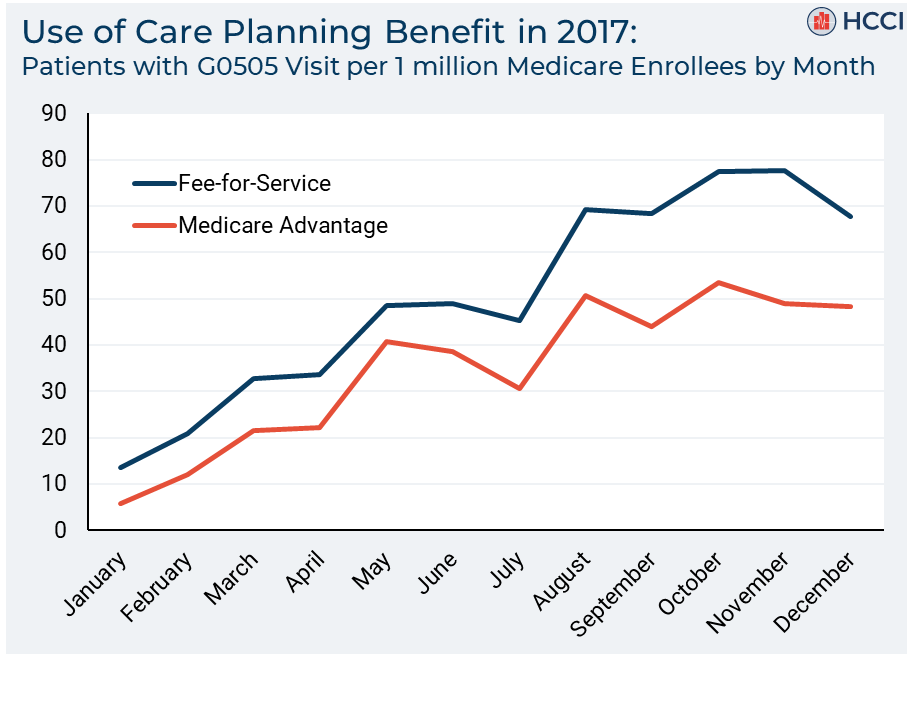
Examining the adoption of a new Medicare billing code for cognitive assessments: a slow but steady uptake
 Read more: Examining the adoption of a new Medicare billing code for cognitive assessments: a slow but steady uptake
Read more: Examining the adoption of a new Medicare billing code for cognitive assessments: a slow but steady uptakeOn January 1, 2017, the Medicare program started reimbursing providers for a new procedure code for clinical visits for cognitive assessments and care planning services (CPT code G0505). This newly-billable service is intended to improve the care of patients with Alzheimer’s disease and related dementias and hopefully increase early detection and diagnosis. A G0505 visit…
-
Los Angeles Times: Health Insurance Deductibles Soar, Leaving Americans with Unaffordable Bills
 Read more: Los Angeles Times: Health Insurance Deductibles Soar, Leaving Americans with Unaffordable Bills
Read more: Los Angeles Times: Health Insurance Deductibles Soar, Leaving Americans with Unaffordable BillsHCCI’s research on consumer-directed health plans was recently used to support the first in a series of articles by the Los Angeles Times on high-deductible health plans. From the article: “The challenges are most severe for people with the highest deductibles, according to the poll: Nearly half of those in a plan with at least…
-
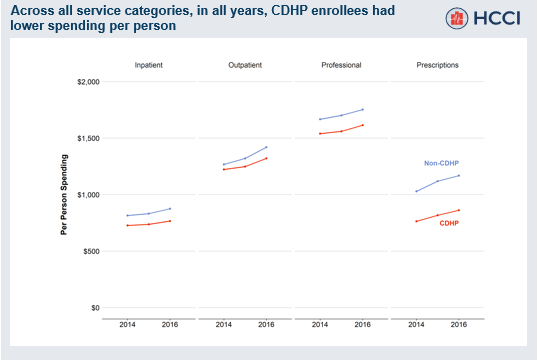
Lower Health Care Spending and Use for People with Chronic Conditions in Consumer-Directed Health Plans
Read more: Lower Health Care Spending and Use for People with Chronic Conditions in Consumer-Directed Health PlansTo better understand differences in spending and use across types of health plans, we examine individuals enrolled in consumer-directed health plans (CDHPs) and individuals enrolled in non-CDHP health plans. CDHPs are a type of HDHP that typically include a health savings account (HSA) or a health reimbursement arrangement (HRA). We analyzed a sample of over…
-
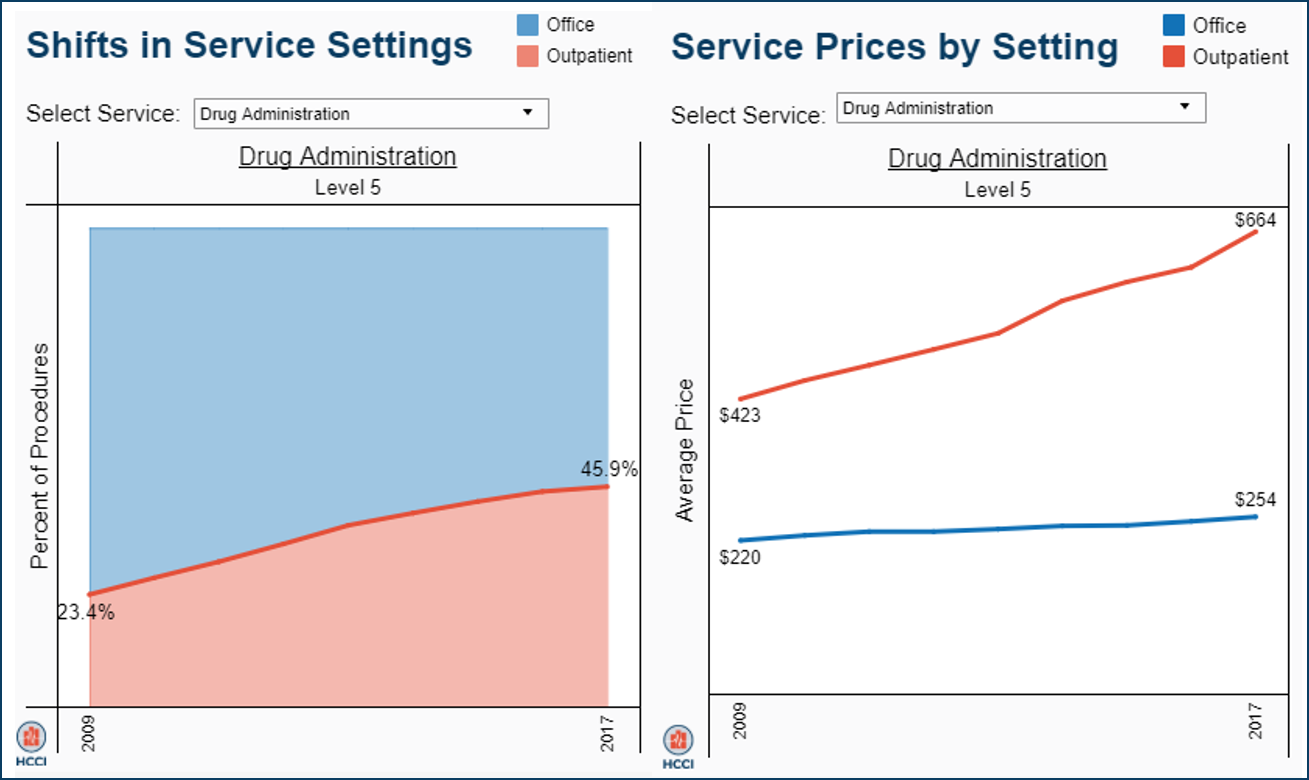
Shifting Care from Office to Outpatient Settings: Services are Increasingly Performed in Outpatient Settings with Higher Prices
 Read more: Shifting Care from Office to Outpatient Settings: Services are Increasingly Performed in Outpatient Settings with Higher Prices
Read more: Shifting Care from Office to Outpatient Settings: Services are Increasingly Performed in Outpatient Settings with Higher PricesWhere people receive health care matters, especially in terms of costs. The same services may have a much higher price tag when performed in one setting rather than another, but this price difference is rarely publicized to patients. To understand what settings people used and how prices differed, we looked at the utilization and average…
-
American Economic Journal: Applied Economics: Health Care Spending and Utilization in Public and Private Medicare
Tags: American Economic Journal: Applied Economics, Medicare, Medicare Advantage, Peer Reviewed Journals, Spending, Utilization Read more: American Economic Journal: Applied Economics: Health Care Spending and Utilization in Public and Private Medicare
Read more: American Economic Journal: Applied Economics: Health Care Spending and Utilization in Public and Private MedicareAbstract: We compare health care spending in public and private Medicare using newly available claims data from Medicare Advantage (MA) insurers. MA insurer revenues are 30 percent higher than their health care spending. Adjusting for enrollee mix, health care spending per enrollee in MA is 9 to 30 percent lower than in Traditional Medicare (TM),…
-
2017 Annual Health Care Cost and Utilization Report Webinar
Tags: Drug Spending, HCCUR, Inpatient Spending, Outpatient Spending, Physician Spending, Prices, Utilization Read more: 2017 Annual Health Care Cost and Utilization Report Webinar
Read more: 2017 Annual Health Care Cost and Utilization Report WebinarHCCI recently held a webinar to discuss the 2017 Annual Health Care Cost and Utilization Report.
-
2017 Health Care Cost and Utilization Report
Tags: Drug Spending, HCCUR, Inpatient Spending, Out-of-Pocket, Outpatient Spending, Physician Spending, Prices, Utilization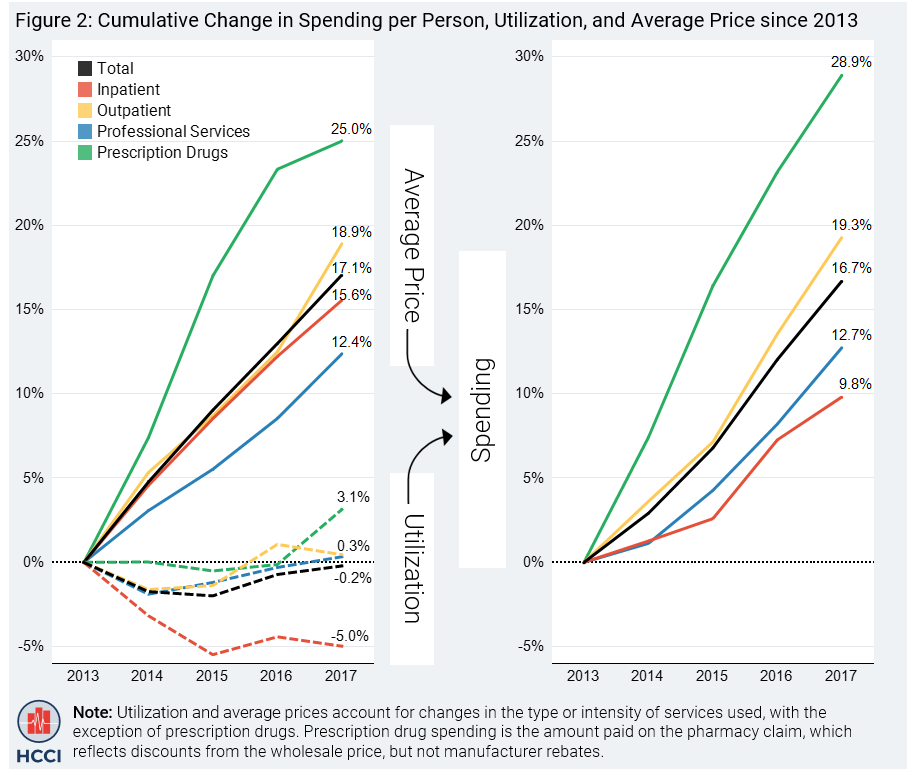 Read more: 2017 Health Care Cost and Utilization Report
Read more: 2017 Health Care Cost and Utilization ReportThe 2017 Health Care Cost and Utilization Report shows that spending per privately insured person grew by 4.2 percent, the second year in a row of spending growth over four percent. Price increases were the primary driver. The report covers the period 2013 through 2017 and includes claims data from four national insurance companies: Aetna, Humana, Kaiser Permanente, and…
-
Trends In Primary Care Visits
 Read more: Trends In Primary Care Visits
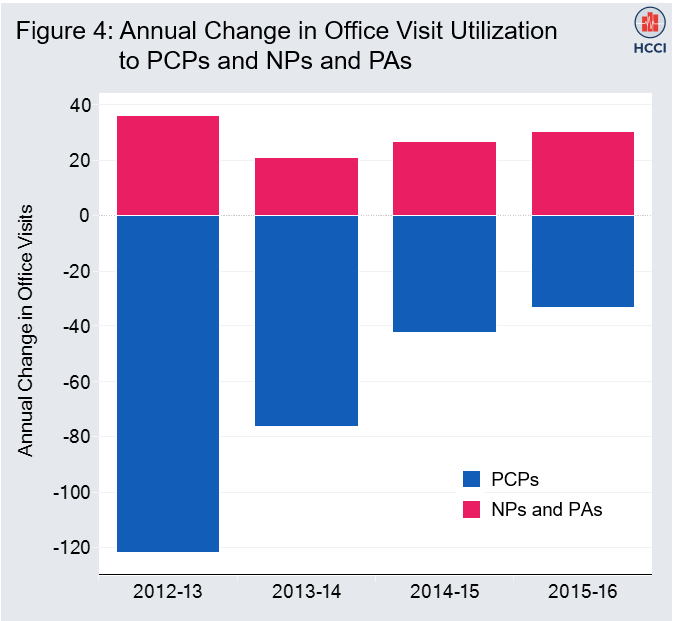
Read more: Trends In Primary Care VisitsOffice visits to primary care physicians (PCPs) declined 18 percent from 2012 to 2016 for adults under 65 years old with employer-sponsored health insurance, while office visits to nurse practitioners (NPs) and physician assistants (PAs) increased 129 percent. Comparing 2012 to 2016, there were 273 fewer office visits per 1,000 insured individuals to primary care…
-
Health Affairs: Assessing The Impact Of State Policies For Prescription Drug Monitoring Programs On High-Risk Opioid Prescriptions
Tags: Commercially Insured, Geographic Variation, Health Affairs, Opioids, Peer Reviewed Journals, Utilization Read more: Health Affairs: Assessing The Impact Of State Policies For Prescription Drug Monitoring Programs On High-Risk Opioid Prescriptions
Read more: Health Affairs: Assessing The Impact Of State Policies For Prescription Drug Monitoring Programs On High-Risk Opioid PrescriptionsABSTRACT: Policies and practices have proliferated to optimize prescribers’ use of their states’ prescription drug monitoring programs, which are statewide databases of controlled substances dispensed at retail pharmacies. Our study assessed the effectiveness of three such policies: comprehensive legislative mandates to use the program, laws that allow prescribers to delegate its use to office staff,…
-
2016 Health Care Cost and Utilization Report
Tags: Drug Spending, Geographic Variation, HCCUR, Inpatient Spending, Out-of-Pocket, Outpatient Spending, Physician Spending, Prices, Utilization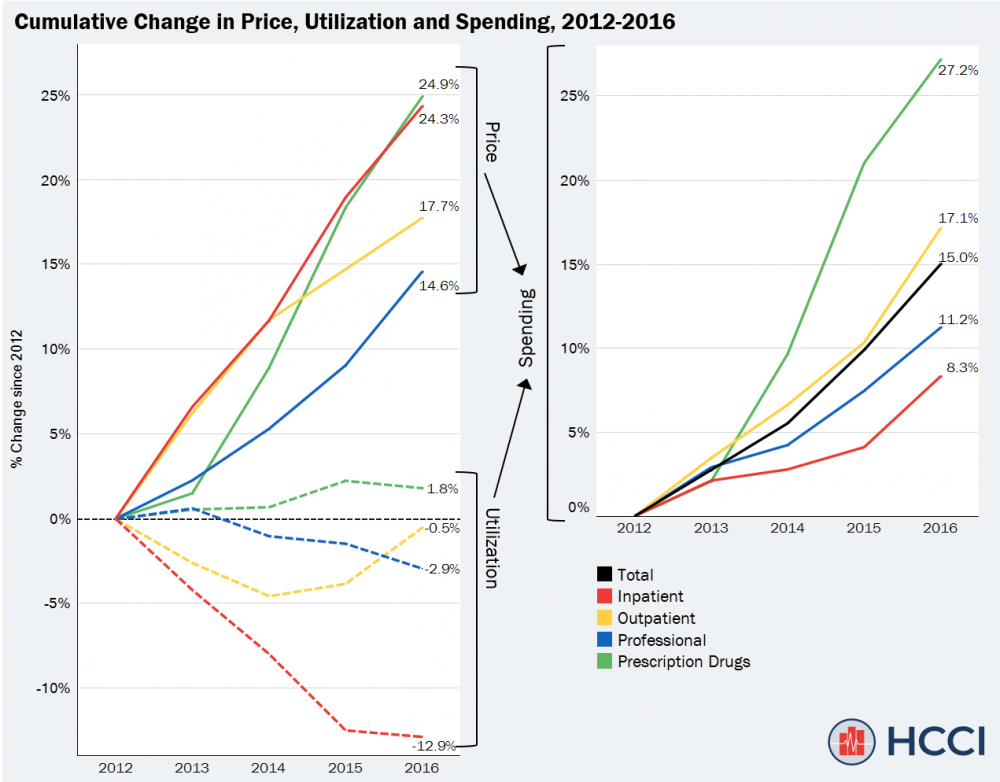 Read more: 2016 Health Care Cost and Utilization Report
Read more: 2016 Health Care Cost and Utilization ReportThe 2016 Health Care Cost and Utilization Report shows that spending per privately insured person grew by 4.6 percent, faster than in previous years. Price increases were the primary driver. The report covers the period 2012 through 2016 and includes claims data from four national insurance companies: Aetna, Humana, Kaiser Permanente, and UnitedHealthcare. The data in…