Surprise Billing
-
JAMA Internal Medicine: Association of Surprise-Billing Legislation with Prices Paid to In-Network and Out-of-Network Anesthesiologists in California, Florida, and New York: An Economic Analysis
Tags: Surprise Billing Read more: JAMA Internal Medicine: Association of Surprise-Billing Legislation with Prices Paid to In-Network and Out-of-Network Anesthesiologists in California, Florida, and New York: An Economic Analysis
Read more: JAMA Internal Medicine: Association of Surprise-Billing Legislation with Prices Paid to In-Network and Out-of-Network Anesthesiologists in California, Florida, and New York: An Economic AnalysisQuestion What is the association of state surprise-billing legislation with prices paid to anesthesiologists in hospital outpatient departments and ambulatory surgery centers? Findings This retrospective economic analysis of more than 2.5 million claims filed for patients with private health insurance who received anesthesia services in hospital outpatient departments and ambulatory surgery centers from 2014 to…
-
Real World Consequences of the Qualifying Payment Amount in the No Surprises Act
Tags: Surprise Billing Read more: Real World Consequences of the Qualifying Payment Amount in the No Surprises Act
Read more: Real World Consequences of the Qualifying Payment Amount in the No Surprises ActThe United States Congress passed the No Surprises Act last year, offering several protections to consumers. Beginning in 2022, providers can no longer bill patients for more than their insurance’s in-network cost sharing. The law also bans balance billing except in situations where a patient is notified in advance and their written consent is obtained….
-
American Journal of Managed Care: Policies to Address Surprise Billing Can Affect Health Insurance Premiums
 Read more: American Journal of Managed Care: Policies to Address Surprise Billing Can Affect Health Insurance Premiums
Read more: American Journal of Managed Care: Policies to Address Surprise Billing Can Affect Health Insurance PremiumsAbstract: Objectives: To quantify the proportion of health plan spending on services for which surprise billing is common—provided by radiologists, anesthesiologists, pathologists, emergency physicians, emergency ground ambulances, and emergency outpatient facilities—and estimate the potential impact of proposed policies to address surprise billing on health insurance premiums. Study Design: Analysis of 2017 commercial claims data from…
-
Health Affairs: Surprise Bills, Benchmarks, And The Problem Of Indexation
 Read more: Health Affairs: Surprise Bills, Benchmarks, And The Problem Of Indexation
Read more: Health Affairs: Surprise Bills, Benchmarks, And The Problem Of IndexationHCCI data was cited in a Health Affairs blog article on surprise billing. From the Article: “Over the past year, the congressional debate over surprise billing has converged on two policy options to resolve out-of-network payments—1) a simple benchmark, in which a health plan pays out-of-network providers the median rate agreed with local in-network providers…
-
How common is out-of-network billing?
Tags: Commercially Insured, Emergency Room, Geographic Variation, Mental Health and Substance Use, Out-of-Network, Surprise Billing Read more: How common is out-of-network billing?
Read more: How common is out-of-network billing?Congress is considering legislation to address “surprise bills”, which occur when a person visits an in-network facility, but receives services from a provider that is outside of their insurer’s network. Bills in both the House and Senate include provisions to determine a benchmark rate for out-of-network payments based on what in-network providers of the same…
-
Health Affairs: Surprise Billing: Choose Patients Over Profit
 Read more: Health Affairs: Surprise Billing: Choose Patients Over Profit
Read more: Health Affairs: Surprise Billing: Choose Patients Over ProfitHCCI’s research on median in-network rates was recently featured in a Health Affairs blog post on surprise billing. From the blog: “Most importantly, Congress should establish a locally based benchmark to determine the amount an insurer would be required to pay a provider for a surprise bill. Ideally, we’d set the benchmark at some multiple…
-
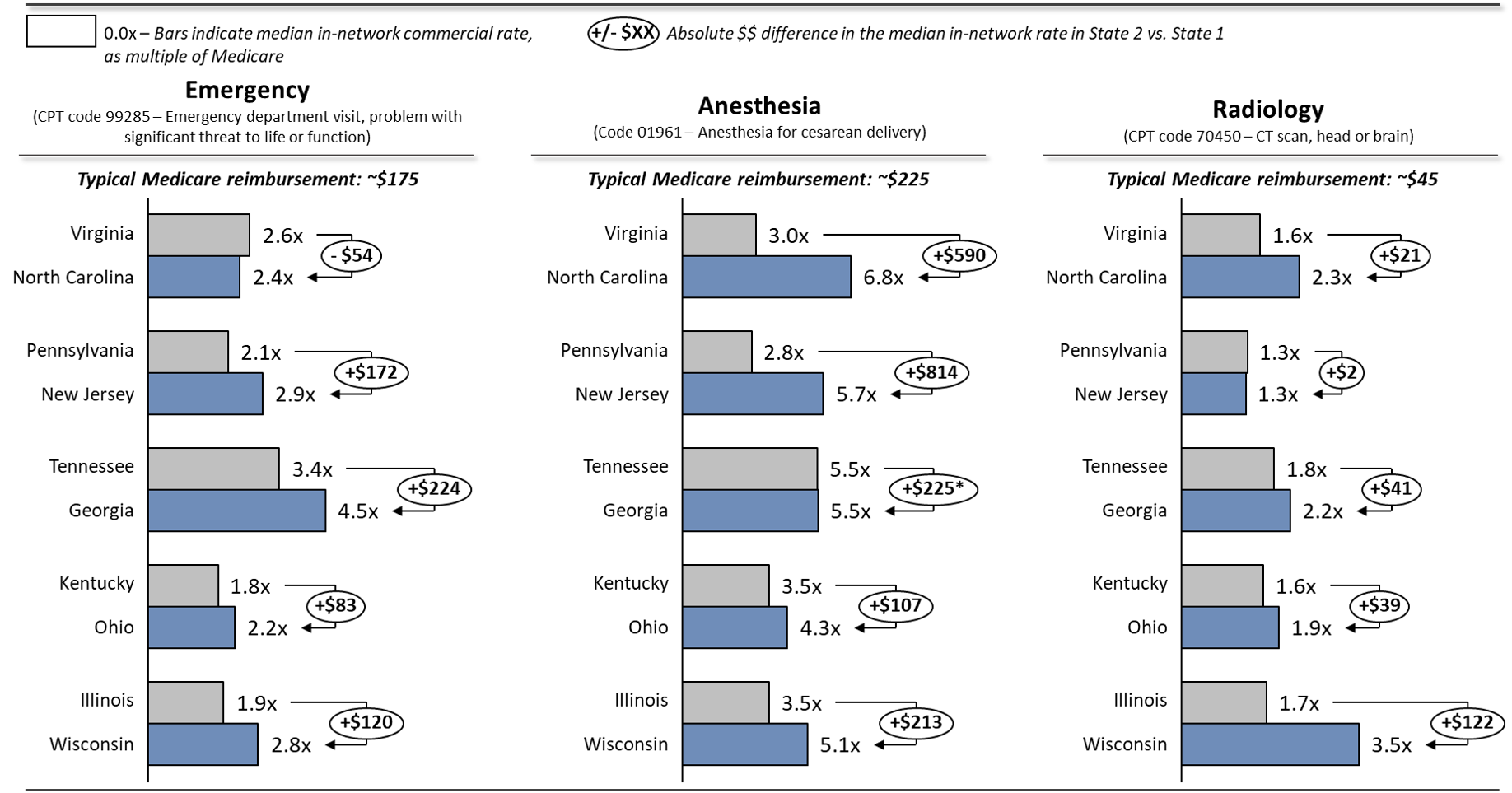
Comparing Commercial and Medicare Rates for Select Anesthesia, Emergency Room, and Radiology Services by State
Tags: Commercially Insured, Emergency Room, Medicare, Physician Spending, Prices, Spending, Surprise Billing Read more: Comparing Commercial and Medicare Rates for Select Anesthesia, Emergency Room, and Radiology Services by State
Read more: Comparing Commercial and Medicare Rates for Select Anesthesia, Emergency Room, and Radiology Services by StateCommittees in both the House and Senate have advanced legislation that includes measures to address “surprise bills.” A surprise bill results when a person unknowingly receives medical care from a provider that is not part of their insurer’s network. Both pieces of legislation set a benchmark for out-of-network payments. Those benchmarks are determined based on…
-
CBS Evening News: Family Hit With $3,700 Bill For Out-Of-Network Anesthesiologist
 Read more: CBS Evening News: Family Hit With $3,700 Bill For Out-Of-Network Anesthesiologist
Read more: CBS Evening News: Family Hit With $3,700 Bill For Out-Of-Network AnesthesiologistHCCI’s research on out-of-network billing was recently cited by a CBS Evening News report on the topic. Family hit with $3,700 bill for out-of-network anesthesiologist – CBS News When Adam and Laura Parkinson chose their hospital and obstetrician for the birth of their son, they didn't think they would get hit with a surprise bill…
-
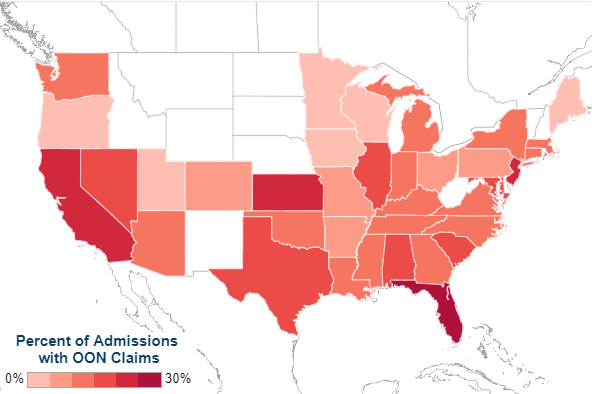
Surprise out-of-network medical bills during in-network hospital admissions varied by state and medical specialty, 2016
Read more: Surprise out-of-network medical bills during in-network hospital admissions varied by state and medical specialty, 2016Out-of-network billing practices have increasingly garnered attention as individuals with commercial health insurance continue to experience “surprise billing.” A surprise medical bill commonly describes a charge to a patient for care delivered by an out-of-network (OON) professional who works within an in-network facility. We used the Health Care Cost Institute’s (HCCI) vast commercial claims database to…