Mental Health and Substance Use
-
Mental Health Service Use Among People with Employer-Sponsored Insurance
 Read more: Mental Health Service Use Among People with Employer-Sponsored Insurance
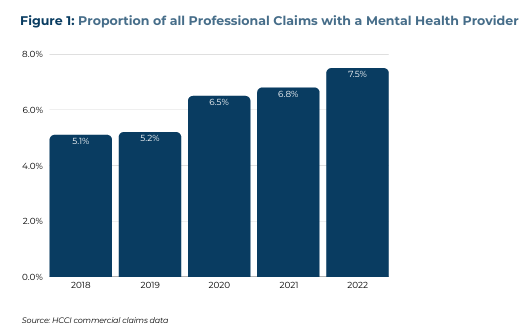
Read more: Mental Health Service Use Among People with Employer-Sponsored InsuranceThe Health Care Cost Institute (HCCI), in collaboration with West Health, conducted an analysis on the use of office-based mental health services among people with employer-sponsored insurance (ESI). We found that use of mental health services has increased from 2018-2022, and that therapy was the most commonly used service. We found an increase in spending…
-
Telehealth Access is Crucial to Mental Health Care for People with Employer-Sponsored Insurance
 Read more: Telehealth Access is Crucial to Mental Health Care for People with Employer-Sponsored Insurance
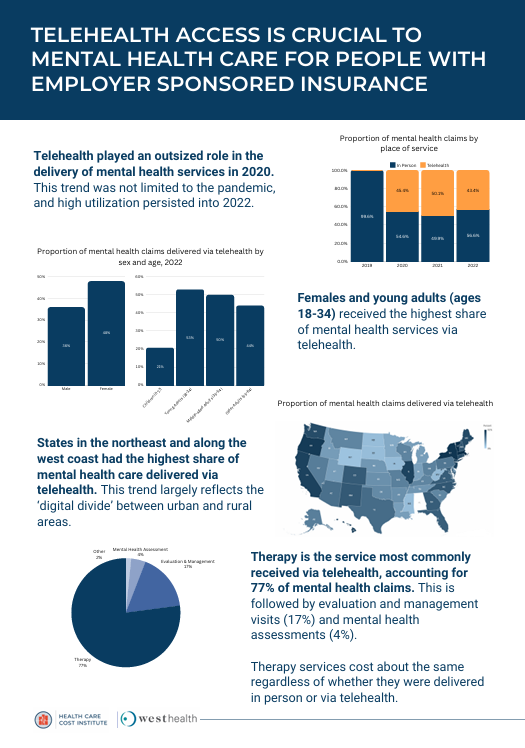
Read more: Telehealth Access is Crucial to Mental Health Care for People with Employer-Sponsored InsuranceThe Health Care Cost Institute (HCCI), in collaboration with West Health, conducted an analysis on the use of telehealth mental health services among people with employer-sponsored insurance (ESI). We found that telehealth played an outsized role in the delivery of mental health services starting in 2020, with over 40% of mental health visits occurring via telehealth from…
-
Vox: Her son died after insurers resisted covering drug rehab. Now she’s taking them to court.
 Read more: Vox: Her son died after insurers resisted covering drug rehab. Now she’s taking them to court.
Read more: Vox: Her son died after insurers resisted covering drug rehab. Now she’s taking them to court.HCCI data was used in an article about the cost of substance use disorder rehab. From the article: “Insurers do seem to be paying more for addiction care than they used to. According to the Health Care Cost Institute, commercial insurers spent a little more than $17,000 on the average patient with a substance use…
-
How common is out-of-network billing?
Tags: Commercially Insured, Emergency Room, Geographic Variation, Mental Health and Substance Use, Out-of-Network, Surprise Billing Read more: How common is out-of-network billing?
Read more: How common is out-of-network billing?Congress is considering legislation to address “surprise bills”, which occur when a person visits an in-network facility, but receives services from a provider that is outside of their insurer’s network. Bills in both the House and Senate include provisions to determine a benchmark rate for out-of-network payments based on what in-network providers of the same…
-
Antidepressant Use Increased for Individuals with a Mood Disorder with Employer-Sponsored Insurance
 Read more: Antidepressant Use Increased for Individuals with a Mood Disorder with Employer-Sponsored Insurance
Read more: Antidepressant Use Increased for Individuals with a Mood Disorder with Employer-Sponsored InsuranceDepression is a common mood disorder that affects how people feel, think, and conduct daily activities. Approximately 17 million adults (1 in 14) had at least one major depressive episode in 2017. Surveys have found that antidepressant prescribing has increased over the past two decades. For example, a 2017 National Center for Health Statistics survey found that,…
-
Health Affairs: Medicare Advantage And Commercial Prices For Mental Health Services
Tags: Commercially Insured, Health Affairs, Medicare Advantage, Mental Health and Substance Use, Peer Reviewed Journals Read more: Health Affairs: Medicare Advantage And Commercial Prices For Mental Health Services
Read more: Health Affairs: Medicare Advantage And Commercial Prices For Mental Health ServicesAbstract: In 2014, insurers paid an average of 13–14 percent less for in-network mental health services in their commercial and Medicare Advantage plans than fee-for-service Medicare paid for identical services—despite paying up to 12 percent more than Medicare when the same services were provided by other physician specialties. However, patients went out of network more…
-
Doctors Lounge: Socioeconomic Factors Associated With Opioid Prescriptions
 Read more: Doctors Lounge: Socioeconomic Factors Associated With Opioid Prescriptions
Read more: Doctors Lounge: Socioeconomic Factors Associated With Opioid PrescriptionsAmong disabled Medicare beneficiaries, county-level socioeconomic factors are associated with opioid prescriptions, with more prescriptions seen with lower socioeconomic indicators, according to a study published in the January issue of Medical Care. Chao Zhou, Ph.D., from the Health Care Cost Institute in Washington, D.C., and colleagues examined opioid prescriptions of disabled Medicare beneficiaries without record…
-
Psychiatric Services: Telehealth Delivery of Mental Health Services: An Analysis of Private Insurance Claims Data in the United States
 Read more: Psychiatric Services: Telehealth Delivery of Mental Health Services: An Analysis of Private Insurance Claims Data in the United States
Read more: Psychiatric Services: Telehealth Delivery of Mental Health Services: An Analysis of Private Insurance Claims Data in the United StatesABSTRACT: Objective: This study characterizes telehealth claims for mental health and substance abuse (MH/SA) services by using national private claims data. Methods: Telehealth-related mental health service claims were identified with private claims data from 2009 to 2013. These data—provided by the Health Care Cost Institute—included claims from Aetna, Humana, and UnitedHealth for more than 50 million individuals…
-
Selected Health Care Trends for Young Adults: 2007-2012
Tags: Affordable Care Act, Emergency Room, Inpatient Spending, Mental Health and Substance Use, Outpatient Spending Read more: Selected Health Care Trends for Young Adults: 2007-2012
Read more: Selected Health Care Trends for Young Adults: 2007-2012This issue brief is one of the first to examine health care trends for young adults (ages 19-25) with employer-sponsored insurance before and after implementation of Section 1001 of the Affordable Care Act that allows parents to include their adult children in family health plans.
-
Children’s Health Spending: 2009-2012
 Read more: Children’s Health Spending: 2009-2012
Read more: Children’s Health Spending: 2009-2012The Children’s Health Care Spending: 2009-2012 report shows that spending on health care for privately insured children increased between 2009 and 2012, rising an average 5.5 percent a year, with more dollars spent on boys than girls, and higher spending on infants and toddlers (ages 0-3) than any other children’s age group. Key Findings…
