All HCCI Reports
HCCI’s original reports powered by #HCCIdata
-
Charge Amounts for Professional Procedures to Commercial Insurance and Traditional Medicare
 Read more: Charge Amounts for Professional Procedures to Commercial Insurance and Traditional Medicare
Read more: Charge Amounts for Professional Procedures to Commercial Insurance and Traditional MedicareIn the start of 2019, Centers for Medicare and Medicaid Services finalized federal policies that required hospitals to publish the amount they charge for common services, documents commonly referred to as chargemasters. While similar policies have been in place at the state level since the early 2000s, this was the first federal mandate to require…
-
ADRD Prevalence in Various Insurance Populations: A Collaboration with The Alzheimer’s Association
 Read more: ADRD Prevalence in Various Insurance Populations: A Collaboration with The Alzheimer’s Association
Read more: ADRD Prevalence in Various Insurance Populations: A Collaboration with The Alzheimer’s AssociationAlzheimer’s disease and related dementias (ADRD) represent a significant and growing cost to the United States health care system. While the prevalence and cost of ADRD related to Medicare Fee-for-Service beneficiaries is documented in the Center for Medicare and Medicaid Services’ Chronic Conditions Warehouse, less is known about the prevalence and cost of ADRD among…
-
Impact of New Technology on Prices and Use: A Case Examination of Robot-Assisted Surgeries
 Read more: Impact of New Technology on Prices and Use: A Case Examination of Robot-Assisted Surgeries
Read more: Impact of New Technology on Prices and Use: A Case Examination of Robot-Assisted SurgeriesSurgery accounts for the largest share of inpatient and outpatient spending among individuals with employer-sponsored insurance, representing 49 percent of inpatient spending and 37 percent of outpatient spending in 2018 according to HCCI’s most recent annual report. In recent years, the number of surgical procedures performed using robot assistance has increased dramatically. Intuitive, Inc., which…
-
Consumer-Directed Health Plan Enrollment Rises in All Cities over 10 Years (2008 to 2017)
Tags: 10 Year Trend, Commercially Insured, Consumer-Directed Health Plans, Geographic Variation, Out-of-Pocket, Spending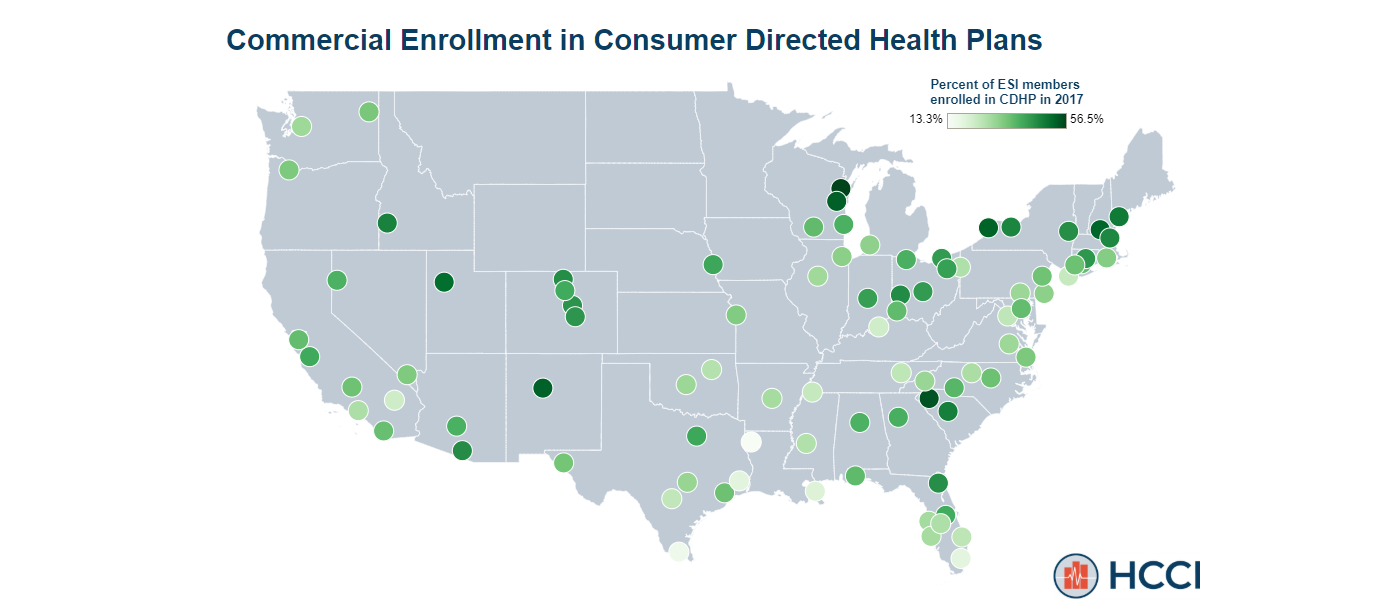 Read more: Consumer-Directed Health Plan Enrollment Rises in All Cities over 10 Years (2008 to 2017)
Read more: Consumer-Directed Health Plan Enrollment Rises in All Cities over 10 Years (2008 to 2017)Recent analysis by HCCI finds that enrollment in consumer-directed health plans (CDHPs) increased dramatically since 2008. Nationally, nearly a third of commercially insured individuals were enrolled in a CDHP in 2017, up from 7.5% in 2008. Over ten years, enrollment in CDHPs doubled in 85 of the 88 metro areas studied. High-deductible health plans (HDHPs) have become increasingly common…
-
Health Affairs Blog: Out-of-Network Spending: Why Growing Attention Is Focused On A Small Share Of Medical Spending
Tags: Out-of-Network Read more: Health Affairs Blog: Out-of-Network Spending: Why Growing Attention Is Focused On A Small Share Of Medical Spending
Read more: Health Affairs Blog: Out-of-Network Spending: Why Growing Attention Is Focused On A Small Share Of Medical SpendingIn HCCI’s publication in Health Affairs Blog, we examine the cost and utilization of out-of-network care in commercial claims. From the article: “People receiving surprise bills, sometimes totaling tens of thousands of dollars, have been frequently chronicled by high-profile media stories and in academic research over the past several years. Previous research from the Health Care Cost…
-
Health Affairs: Out-Of-Network Spending Mostly Declined In Privately Insured Populations With A Few Notable Exceptions From 2008 To 2016
Tags: Out-of-Network Read more: Health Affairs: Out-Of-Network Spending Mostly Declined In Privately Insured Populations With A Few Notable Exceptions From 2008 To 2016
Read more: Health Affairs: Out-Of-Network Spending Mostly Declined In Privately Insured Populations With A Few Notable Exceptions From 2008 To 2016In HCCI’s publication in Health Affairs, we examined out-of-network spending in the privately insured population. Abstract: “While out-of-network or potential “surprise” billing has garnered increasing attention, particularly in emergency department and inpatient settings, few national studies have examined out-of-network care overall or in other settings. We examined out-of-network spending and use among two large nationwide…
-
How often do providers bill out of network?
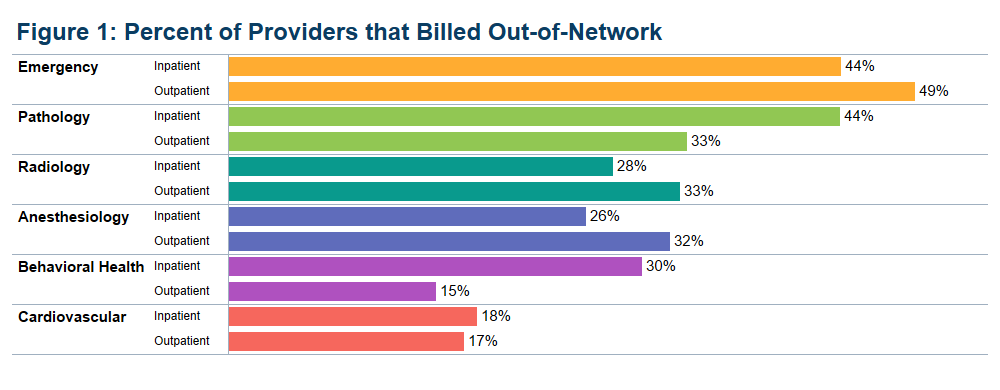 Read more: How often do providers bill out of network?
Read more: How often do providers bill out of network?In recent analysis, we document extensive variation across states and metropolitan areas in the frequency of out-of-network visits among individuals with health insurance provided by an employer. These differences raise the question of whether individual providers bill out of network at dissimilar rates. To explore whether a small group of providers are responsible for most…
-
Use of Prenatal Care Varies among People with Employer-Sponsored Insurance
Tags: Maternal HealthRead more: Use of Prenatal Care Varies among People with Employer-Sponsored InsurancePrenatal care leads to healthier pregnancy, healthier pregnant people, and healthier babies. In fact, birthing parents who receive prenatal care are three times less likely to deliver low birthweight babies, and the baby is five times more likely to survive delivery. To explore the kind of prenatal care pregnant people receive, we looked at utilization…
-
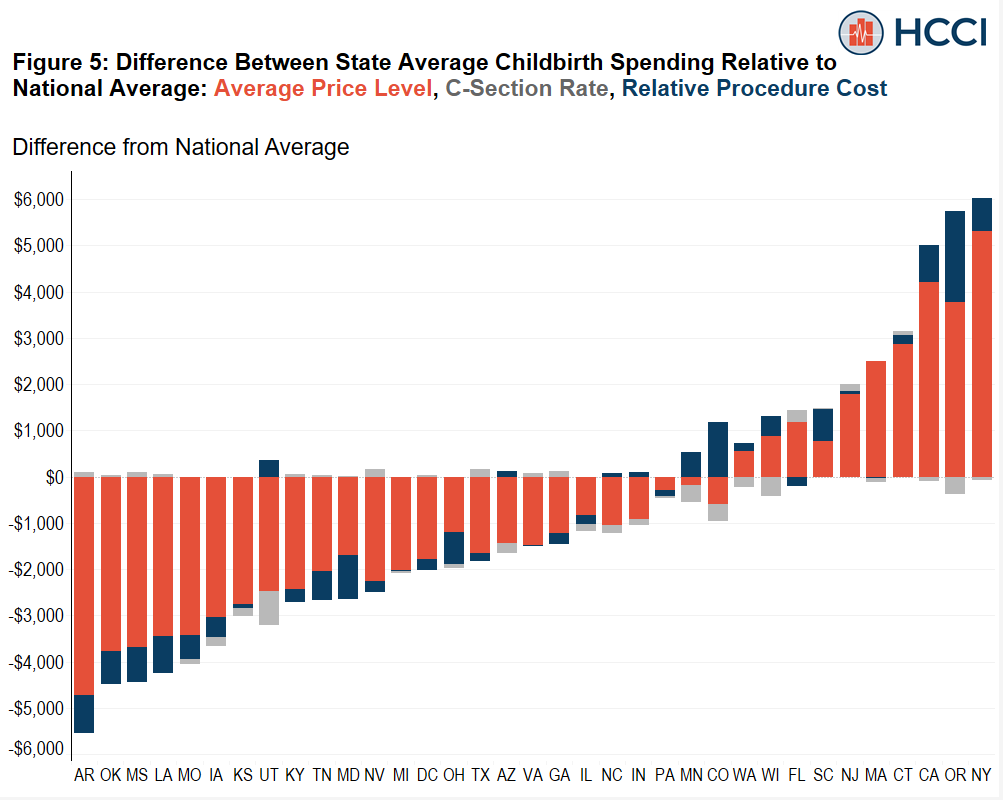
Understanding Variation in Spending on Childbirth Among the Commercially Insured
Read more: Understanding Variation in Spending on Childbirth Among the Commercially InsuredChildbirth is the most frequent reason for an inpatient admission in the United States, and Cesarean-section (C-section) is the most common operating room procedure in an inpatient hospital stay. Among people who get insurance through an employer, the combination of labor, delivery, and newborn care makes up nearly one in six dollars spent on inpatient…
-
Most Postpartum Spending Occurs Beyond 60 Days After Delivery
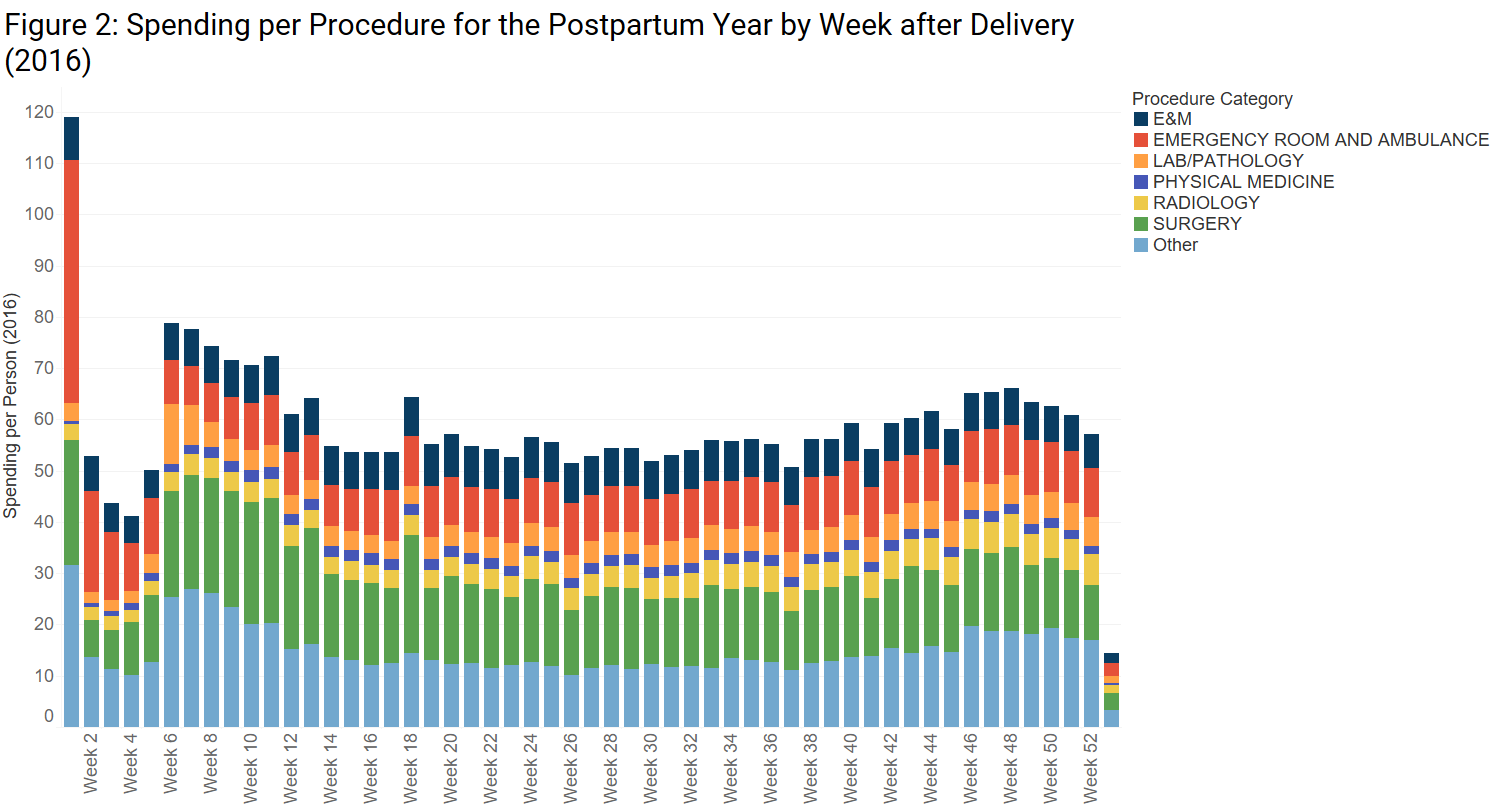 Read more: Most Postpartum Spending Occurs Beyond 60 Days After Delivery
Read more: Most Postpartum Spending Occurs Beyond 60 Days After DeliveryThe postpartum period is a vulnerable time for both birthing parent and newborn and is critically important to their health and well-being. The American College of Obstetricians and Gynecologists (ACOG) recommends ongoing, comprehensive care, including physical, social, and psychological services, during the postpartum period. In large part because of an increasing maternal mortality rate in the US –…